Estimated read time: 4-5 minutes
- Neal Meredith faced $80,000 in medical bills despite being assured coverage.
- His insurance company misclassified the hospital as in-network, later admitting the mistake.
- Federal laws protect emergency patients, but not in non-emergent situations.
ELK RIDGE, Utah County – Last summer, Neal Meredith had blood clots in his legs.
"'We need to get you in now,'" Meredith said doctors told him. "'It's urgent enough. It's an emergency.'"
But even facing medical care with life-threatening urgency, Meredith took a beat to dot his I's and cross his T's with his insurance.
"We want to make sure it's covered," he said.
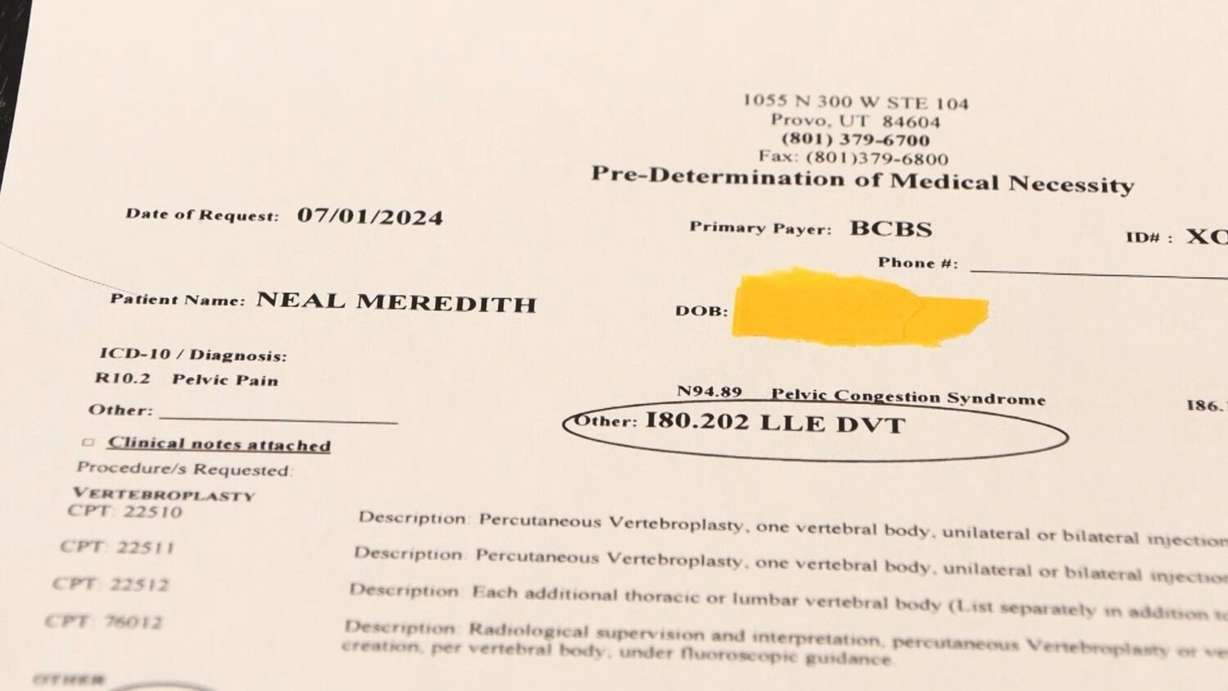
He was assured he had coverage. On a "Pre-Determination of Medical Necessity" form, a representative for his insurance company determined, "Authorization Not Needed."
"What does that mean to you?" I asked Meredith.
"That means it's not needed to get it done," he answered.
Authorization not needed
Meredith needed two procedures, and he got the same "Authorization Not Needed" determination for each. For the second one, he even received direct assurance that his coverage was good. A hospital representative sent him a text saying, "We did call your insurance again today and they verified you ARE in-network with this hospital, and there is no preauthorization required for this procedure."
That turned out not to be the case. Meredith's insurance company said the hospital is not in network, and he owed the hospital nearly $80,000.
"You went to the trouble of asking this question before you had the procedure and you're still getting these bills?" I asked Meredith.
"Yes," Meredith replied.
"That doesn't seem fair," I said.
"No," Meredith answered. "And they made slight changes in the last couple of months to find more bills to add on to."
Meredith said his protests with his insurance company and the hospital went nowhere. He said he doesn't have that kind of money. He could declare bankruptcy, but lawyers told him that would likely cost him his house.
"So, what are you going to do?" I asked him.
"So far – fight," Meredith responded. "Anywhere I can."
To that end, Neal decided it was time to call me.
I began by reaching out to Meredith's insurance company, Blue Cross Blue Shield of Illinois, to ask how they can refuse to pay after they informed the hospital that authorization was not needed? I heard back from a spokesperson, who would only tell me they have no comment for this report, citing privacy reasons.
Major medical bill adjustment
I also reached out to the hospital, Utah Valley Hospital in Provo, asking about the massive charges they were passing onto Meredith.
An Intermountain hospital spokesperson wrote: "Utah Valley Hospital believed the procedure would be considered in-network coverage based on communication with representatives at Blue Cross Blue Shield."
The spokesperson added that, in the time since the denial, the insurance company has covered some of the cost of the procedures.
And, good news for Meredith, the hospital spokesperson said the remaining amount was being written off and his "balance owed is zero."
But this is not where Meredith's story ends.

Insurance regulators step in
He also filed a complaint with the Department of Insurance for the state of Illinois, where his insurance company is based.
After review, the insurance company told Illinois regulators that it messed up. The insurance company admitted that its representative said, "Utah Valley Hospital was in-network."
The response continues, "Due to this inaccurate information being provided," the claim was "being reprocessed."
Federal law protects emergency patients
At the center of all this seems to be confusion over whether the medical services Meredith received were truly an emergency. After driving to the E.R., he was permitted to drive home and return for scheduled surgery the next day.
Utah Valley Hospital's spokesperson writes, "Since the procedures were scheduled on a day different than the initial emergency room visit, Blue Cross Blue Shield eventually denied emergency coverage."
In an emergency, federal law provides protections for patients who seek emergency care at out-of-network hospitals.
Under the Affordable Care Act, insurance companies are required to cover emergency services without prior authorization and at the same cost-sharing rates as in-network care, regardless of whether the hospital is in the patient's network.
Additionally, the No Surprises Act prohibits balance billing in most emergency situations, meaning the patient cannot be charged the difference between the hospital's billed charges and the insurer's payment.
These laws ensure patients are not penalized financially for seeking critical, life-saving care during emergencies, but do not protect patients when the situation is deemed not-emergent.

Photos

Show All 2 Photos














