Estimated read time: 4-5 minutes
MURRAY — Intermountain Medical Center in Murray has become the first U.S. hospital to perform a minimally invasive surgery outside of clinical trials to treat aortic aneurysm using a new FDA-approved device.
"It's a game-changer," said Dr. Evan Brownie, a vascular surgeon at Intermountain Medical Center, who has now implanted the Gore EXCLUDER Thoracoabdominal Branch Endoprosthesis (TAMBE) device multiple times. The endoprosthesis can be used with some aortic aneurysms to avoid a major surgery that normally uses an incision he likens to opening a can of cinnamon rolls because the patient's side is cut from the shoulder blade to the lower abdomen in a very significant operation. The hospital stay itself can exceed two weeks, while full recovery takes a couple of months.
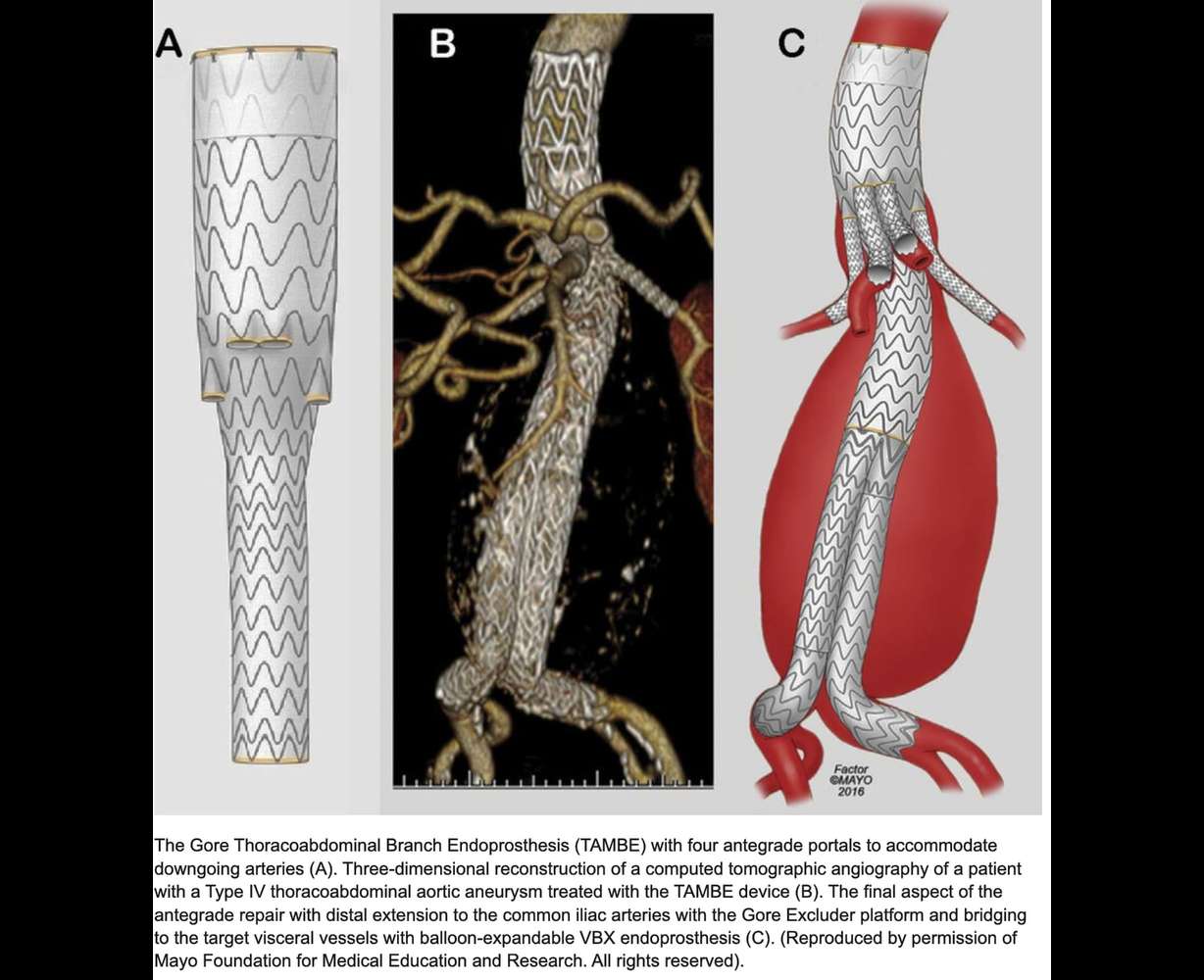
The new procedure instead involves small punctures to the femoral arteries in the groin and one beneath the collarbone to deliver a stent graft which includes small branches that supply blood to impacted organs. A graphic provided to Deseret News by Intermountain Health depicts the device, with its straw-like branches. The endoprosthesis seals off the aneurysm while allowing blood to flow through the four built-in branches that hook into visceral arteries and perfuse the abdomen's organs. Recovery varies, but the hospital stay can be as short as a day or two.
Two of the branches go to the renal arteries to provide blood to the kidneys, the others to the superior mesenteric artery to feel the intestine and colon and the celiac artery to supply blood to the stomach, liver and spleen, Brownie said.
"That's why this is revolutionary, because it has been difficult to come up with an off-the-shelf device in which you could provide blood flow to all of those key structures and still be able to kind of bridge the gap between the chest and the abdomen. That's what this device does," he said.
In a news release, Intermountain said the device "also eliminates the need for physicians to modify existing devices or use off-label techniques, which had been a common practice for over a decade due to the lack of approved options." Efforts to customize devices or develop novel methods, while often successful, made outcomes unpredictable.
Brownie said the approved device, which he has now used a half-dozen times, has yielded excellent results. But he noted that surgeons still need to consider each patient's unique situation when determining how to operate.
Often-deadly aortic aneurysms
Brownie said there are three types of aortic aneurysms, which are weak bulges in the aorta that can burst with deadly results. Such an aneurysm in the chest is called thoracic, while one in the abdomen is abdominal. Thoracoabdominal aortic aneurysms span both the chest and abdomen. Abdominal aneurysm is more common.
Any aortic aneurysm increases the risk that a tear, called an aortic dissection, will occur in the inner layer of the aorta's wall and allow blood to leak. A rupture means the aneurysm has burst, and blood pours out. Aneurysms are so dangerous in part because a tear or leak may be the first symptom.
The Centers for Disease Control and Prevention reported that aortic aneurysms killed just under 10,000 people in the U.S. in 2019, and 6 in 10 of those who died were men. Smoking is a major risk factor for abdominal aortic aneurysms, accounting for three-fourths of those. The link is strong enough that the U.S. Preventive Services Task Force suggests men ages 65 to 75 who ever smoked be screened using ultrasound for the abdominal type, whether they have symptoms or not. High blood cholesterol and hardening of the arteries also heighten risk.
Abdominal aortic aneurysms are most common in men and adults 65 and older. They are also more common for white people than Black people, per the CDC. This type of aneurysm is most often caused by atherosclerosis but can trace to infection or injury. And they are less likely to have symptoms. If they do, it's apt to be throbbing or deep pain in the back or side or in the buttocks, groins or legs.
Thoracic aortic aneurysms are equally common in men and women, the likelihood increasing with age. High blood pressure or sudden injury, as well as certain illnesses, raise the risk.
The National Institutes of Health says symptoms of aortic aneurysm, if any, can include:
- Having a hard time or pain swallowing.
- Difficulty breathing.
- Feeling full without eating much.
- Hoarseness.
- Pain in the area where the aneurysm is located, from the neck down.
- Pulsating or throbbing in the stomach area.
- Shortness of breath.
- Swelling of the face, neck or arms.
People who know they have an aneurysm are warned to watch for symptoms of a tear, which can include feeling light-headed, having a rapid heart rate and sudden, severe pain in the stomach area, chest or back, NIH warns.